Early in the morning, Sunita Sahu turned over with some effort and asked, “Where are the children?” Her husband Bodhram said they were asleep. She sighed. It had been a sleepless night for her. And that worried Bodhram. He had often joked to her that she could fall asleep anytime, anywhere.
But on the night of April 28, as Bodhram and Sunita Sahu’s three sons (ages ranging from 12 to 20) took turns to massage their mother’s arms, legs, head and stomach with warm mustard oil, she groaned in pain. “Something is happening to me,” she mumbled – these are Bodhram’s recollections of the morning.
The Sahu family lives in a shanty in Khargapur Jagir in Lucknow district. They had moved to this village in Chinhat block over two decades ago from their village, Maro, in Bemetra district of Chhattisgarh. Bodhram, 42, works as a mason on construction sites; Sunita, 39, was a homemaker.
April was the month when the second wave of the Covid-19 pandemic had severely hit Uttar Pradesh. On April 24, the state recorded 38,055 new infections – its highest ever, though there have been concerns that UP has underreported the numbers.
“The actual number of cases could be four to five times higher. There is underreporting because people are not coming forward for tests due to the stigma. It is difficult to get the real picture,” says Rashmi Kumari, assistant professor, department of Community Medicine at the Ram Manohar Lohia Institute of Medical Sciences (RMLIMS), Lucknow.
The Sahus are sure that Sunita did not have Covid-19 because no one else in the family had it, though she had fever, body ache and diarrhoea – symptoms that are indicative of the coronavirus.

Bodhram Sahu's wife Sunita was diagnosed with typhoid but could have been Covid-positive too
On the morning of April 26, when she first complained of pain and weakness, Bodhram placed her on the carrier of his cycle and pedalled to a doctor three kilometres away. He asked the doctor if she needed hospitalisation.
Bodhram recalls that the doctor told him: "‘Where will you take her? There is no space in any hospital. Give her these medicines, she will be fine in three days." The doctor called a nearby pathology lab to collect her blood sample. She was not tested for Covid-19.
The test cost Sahu Rs. 3,000. He paid a further Rs. 1,700 for the consultation and a batch of medicines – tablets and capsules taken out of their wrappers and packed in brown paper pouches, and a bottle of a dark brown liquid – for strength, as the doctor explained.
That evening, at 5 p.m., Bodhram pedalled back to the clinic with Sunita despite her protestations that she was too weak. By then the report of her blood test was in. It showed a high level of the enzyme serum glutamic oxaloacetic transaminase, indicative of damage to the liver (among other organs). The doctor said Sunita had typhoid. He refused Bodhram’s request that she be administered a drip for strength and insisted that his medicines would cure her in no time.
Though typhoid in itself is also a global health problem, at times, says a research paper , “... the false-positive Widal test [for typhoid] in COVID-19 patients is significant public health issue for developing world…Now typhoid and dengue false-positive… should be interpreted with caution and requires surveillance and continuous follow-up of these patients during COVID-19 pandemic.”
Confirming the need for caution, Pravin Kumar Das, the anaesthesiologist in-charge of RMLIMS’s Covid-19 hospital says, “There is some cross positivity between Covid and typhoid antibodies. In our clinical experience almost 10 per cent of patients test positive for typhoid but actually have Covid.”
Sunita, who had tested positive for typhoid, passed away just half an hour after she asked about her children on the morning of April 29 – barely three days after she had developed fever and other symptoms. Bodhram thought she had finally fallen asleep and placed his hand on her forehead before letting out a cry which woke up their sons. “Just like that she fell asleep forever,” he told me some weeks ago on the phone from his village, while narrating the entire sequence of events and loss.
To cremate Sunita, the family needed a certificate of death. This was provided by Rabila Mishra, the
pradhan
of Khargapur Jagir. In blue ink, he wrote ‘on 29.04.2021 she died in her hut’. There was no mention of cause of death.
And therefore Sunita will not be counted as a Covid casualty. So along with concern about the underreporting of cases in UP and elsewhere, there is global concern that Covid-19 deaths are far in excess of those that are being reported.

Ramvati with her son Rakesh Kumar at her husband Ram Saran’s kiosk: they disbelieve the ‘Covid-19 positive’ notation
“…we are likely facing a significant undercount of total deaths directly and indirectly attributed to COVID-19,” notes the
World Health Organisation
. “The term “excess deaths” describes deaths beyond what would have been expected under “normal” conditions. It captures not only confirmed deaths, but also COVID-19 deaths that were not correctly diagnosed and reported as well as deaths attributable to the overall crisis conditions. This provides a more comprehensive and accurate measure when compared with confirmed COVID-19 deaths alone.”
Of the many such conditions not correctly diagnosed and linked to Covid is an inflammation of the heart tissue. This hinders supply of oxygen and can cause heart attacks.
This is what happened in the Saran family in Meera Nagar village of Mahmudabad block in Sitapur district, some 56 kilometres from Lucknow. On April 22, around noon, 57-year-old Ram Saran experienced a sharp pain. His wife, 56-year-old Ramvati lifts her hand to her heart to point out where this pain was felt.
Ramvati was then in Lucknow – a city that she had moved to with her husband when she was 16 years old. In the Aliganj locality in the north of the city, where the couple lived with their three children, Ram Saran sold water bottles, chips, soft drinks and cigarettes in a kiosk. Some months ago, he had also added face masks to this array of goods.
With the kiosk shut because of the lockdown Ram Saran had often visited his village to check on their ancestral home. The household, meanwhile, had run on Ramvati’s earnings as a domestic worker.
When Ram Saran complained of discomfort, his son Rajesh Kumar, who works as a photocopy machine operator, rushed him to the Community Health Centre in Mahmudabad, some 10 kilometres from their home. The doctor on duty gave Ram Saran two injections.


Ramvati in the colony where she does domestic work. With the kiosk (right) shut during the lockdown, the household had run on her earnings
“By then my father was gasping for breath. The doctor said we only have a small oxygen cylinder here, it will be of no use, so I must take him to the district hospital [around 8 kilometres from the village],” recalls Kumar. An ambulance was called for by dialling 108 (the state’s centralised number for the service). Ram Saran passed away almost as soon as he was shifted to this ambulance – around 2:30 p.m. on April 22.
“He kept saying ‘I will not live’. He was such a healthy man but he lost all his breaths,” says Kumar.
No death certificate was issued and Ram Saran was cremated the same evening in the village. Though the doctor’s prescription written for him at the CHC notes ‘Covid 19 Ag test positive’ he was cremated without any precautions as the family still believes he died of ‘heart fail’.
Ram Saran’s inability to get care at the CHC speaks of the precarious health facilities in the state’s towns and villages – on May 17, a two-judge bench of the Allahabad High Court too commented on these inadequacies.
But it’s not just CHCs or district hospitals that have fallen short during the pandemic. Even in the capital city Lucknow, health infrastructure is inadequate, as the Maurya family realised some months ago.
On April 12, Sunil Kumar Maurya, 41, admitted at the Chinhat hospital, Lucknow, told his nephew Pawan: “I am out of breath. Why are you keeping me in this hospital. I will get better if you take me home.”
About a week before that, Maurya had started running a fever. He also had a cough, but this had been a persistent problem for him so the family did not pay much attention to it. But when he said, “I do not have the strength to walk” his family members were alarmed – recalls 30-year-old Pawan.
The Mauryas live in Chhoti Jugauli, a slum colony in central Lucknow’s Gomtinagar area, home to many migrant families. Sunil Kumar had come here from Birsinghpur village in Jai Singh Pur block of Sultanpur district more than two decades ago. He worked as a building contractor assigning labourers to construction sites.

Rakesh Kumar with a photo of his father Ram Saran on his phone: the family's inability to get care at the CHC speaks of the precarious health facilities in the state’s towns and villages
The densely populated Chhoti Jugauli and its larger namesake Badi Jugauli, spread over 1.5 kilometres, have between them one primary health centre (PHC) and six
anganwadis
.
The Accredited Social Health Activist (ASHA) at one of these says that there have been no awareness camps or distribution of masks and sanitisers in the area since the pandemic began. She does not want to give her name for fear of government action, but is sure that hundreds of residents in this sprawl of some 15,000 people have contracted Covid-19 – but have not been tested or recorded as positive cases.
Of the 1,517 households that she covers, not a single family has reported Covid deaths. “People are dying of cold, cough and fever, but no one wants to get tested," she told me some months ago. "In March 2020 we were asked to survey 50 houses every day to check for patients with symptoms. Now I do not go out as it is too risky. I have formed a group in my area and ask people to update me on the phone.”
So with local health workers not easily available and the doctor at the PHC put on Covid duty elsewhere, when Maurya became ill there was no one to turn to.
Instead, Pawan, a science graduate who works at a doctor’s clinic in Chhoti Jugauli, took his uncle to a nearby private hospital. There they were charged Rs. 500 for an antigen test, which turned up negative. He then took Maurya to the T. S. Misra Medical College and Hospital, around 30 kilometres away, where he was told that the antigen test was not reliable and hence his uncle could not be allotted a bed.
But the doctor on duty at the emergency ward handed him a prescription which listed, among other medicines, Ivermectin, Vitamin C and Zinc – these are usually recommended for Covid-19 symptoms.

Pawan Maurya: the antigen test turned up negative so his uncle Sunil Kumar Maurya could not be allotted a bed
Sunil Maurya’s oxygen level by then had dropped to 80. The family tried two more hospitals but were told that he required a ventilator, which these hospitals did not have. After four hours of running around, when a hospital was finally found that would admit him, Maurya was hooked to an oxygen cylinder. Another test, this time a RT-PCR, was administered.
On April 12, after some hours of laboured breathing, Sunil passed away. The certificate issued by the Lucknow Municipal Corporation (necessary for cremation/burial) listed ‘heart fail’ as the cause of death. The RT-PCR report that came in two days later said he was Covid-19 positive.
“In a week it was all over. The tests failed us,” says Pawan.
“The second wave of the pandemic and meagre financial resources for healthcare have left the urban poor to die without even a proper diagnosis,” says Richa Chandra, a programme manager at the Lucknow-based Vigyan Foundation, which works with urban slums, the homeless and daily wagers. The urban poor, she adds, live with minimal work and social security, a low level of awareness and in congested housing – and now additionally face fear and stigma of being tested and declared Covid positive.
The fear of being tested is compounded by the fact that both antigen and RT-PCR tests can give false negative results.
“There is a cocktail of reasons why RT-PCR tests might give false results,” says Jyotsna Agarwal, the head of department of microbiology at RMLIMS. “The test is based on the principle of amplification of RNA which unlike DNA needs specific conditions to survive [during transportation]. Also, the swab might not be collected correctly, or the kit used might not be ICMR [Indian Council for Medical Research] approved. Antigen tests give rapid results, but do not amplify the RNA, so they are essentially like looking for a needle in a haystack.”


Neither private clinics nor government hospitals would admit Sadrunisha's son Suaib as his Covid test was negative
An RT-PCR test recorded a negative result for 38-year-old Suaib Akhtar of the Garhi Kanuara locality in central Lucknow’s Manaknagar locality.
Akhtar had recovered from chicken pox in the second week of April. He then insisted on fasting for Ramzan (which began on April 13), though his mother, 65-year-old Sadrunisha, asked him not to.
On April 27, Akhtar started coughing and panting. The family took him for a RT-PCR test and a CT-scan at a private pathology lab – which cost Rs. 7,800. While the test was negative, the scan showed ‘viral pneumonia’. But neither private clinics nor government hospitals would admit him as his Covid test was negative. They were all prioritising Covid cases, the beds were all occupied, and other non-emergency services were on hold.
On April 30, Akhtar passed away, unable to breathe despite being hooked to an oxygen cylinder at home that the family had arranged. “He heaved and started to froth from his mouth,” says Sadrunisha.
She describes her son as a “gifted electrician” who had recently received a job offer from Qatar. “Before he could get his visa for the job, death gave him a visa,” she says.
Akhtar was buried in the grounds at Takiya Meeran Shah in Premwati Nagar, around three kilometres from his home. The certificate issued at the grounds does not list a reason for death. Sadrunisha though is sure that her son had Covid-19 because his immunity must have been low due to the bout of chicken pox.
On June 14, 2020, the government of India had issued
a notification
stating “…dead bodies of such suspected COVID cases should be handed over to their relatives immediately and laboratory confirmation of COVID should not be awaited.”
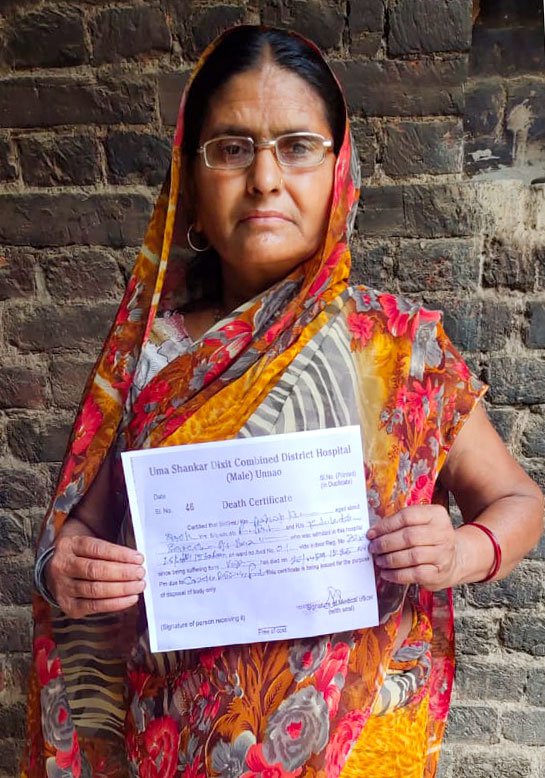

Two days after his death, the family – Vimla and sons Gyanendra Kumar, Dheerendra Kumar and Abhishek – received the test result which said he was Covid-19 positive, but his death certificate (left) says otherwise
This means people who have symptoms but test negative are unlikely to be counted in the list of Covid-19 deaths.
Among them is also Ashok Kumar Yadav, of Qutubuddin Garheva village in Unnao district's Bighapur tehsil . Yadav, a 56-year-old contractual worker in the state’s electricity department, asked the local chemist for medication for the fever and cough he was experiencing since April 22. When the cough worsened and he became weaker, the family took him to the district hospital around 45 kilometres away, on the night of April 25. Yadav was given an RT-PCR test but not admitted. The next day, as he got up from bed to go to the toilet he collapsed on the floor and died.
“Just like that,” says his 51-year-old wife Vimla, a homemaker.
The family – Vimla has three children, ages ranging from 19 to 25 – cremated him without any precautions. Two days later they received the test result which said he was Covid-19 positive. The certificate issued by the district hospital for Yadav lists ‘cardio respiratory failure’ as the cause of death.
“Though we have tried to record all Covid-19 deaths, it is true that tests have not happened in all cases and in some results have come in too late. Now though we are more vigilant about it,” says Girija Shankar Bajpai, an additional director of the state’s health department who oversees Covid-19 management in Lucknow.
Still, how many such cases and deaths have gone unreported, and will never be counted as pandemic casualties – might never be known.
With inputs from Durgesh Singh in Unnao.




