The first-floor room is locked and silent, though it’s well before closing hour. No one is there in an adjacent tin and wood hut either, only a pile of chairs, tables, a metal bench, cartons of iron syrup and folic acid tablets, and discarded wrappings. An old rusted name board also lies there, while a new one at the entrance to the building with the locked room says: ‘Govt. New Type Primary Health Centre, Shabri Mohalla, Dal SGR [Srinagar]’.
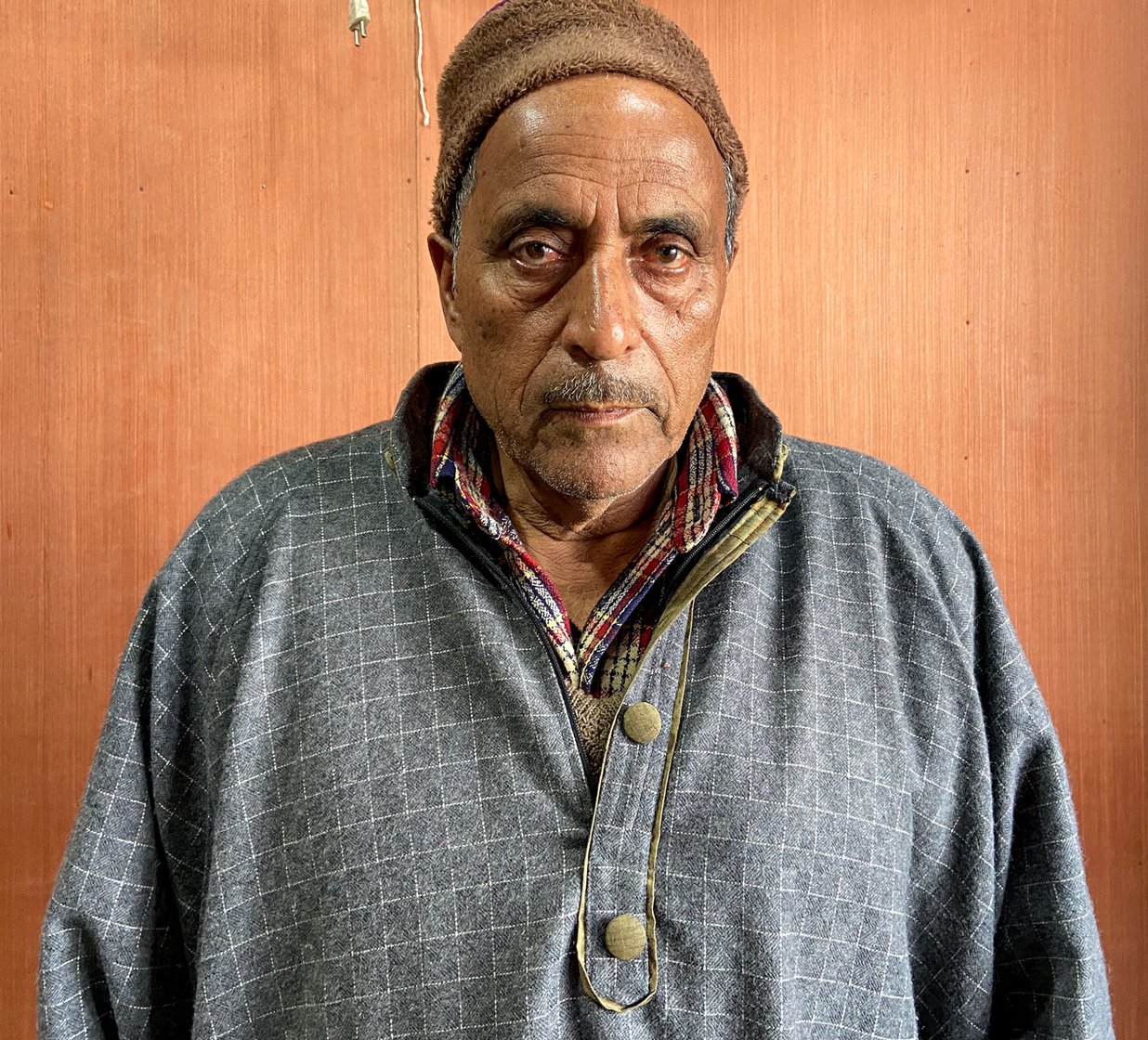
A 10-minute boat ride from here will take you to Nazir Ahmad Bhat’s ‘clinic’, which is usually open – and bustling. On a cold winter afternoon he is meeting his last customer-patient of the afternoon (he will be back in the evening to attend to more) in his small wooden shop on wooden poles, which has a tiny ante-chamber for administering injections. The board outside says ‘Bhat Medicate Chemist and Druggist’.
Hafeeza Dar, around 60 years old, is sitting on a bench here, waiting. She has come to fetch Nazir ‘doctor’ in a boat, her mohalla is a 10-minute ride away. "My mother-in-law has to take some [diabetes] injections and Nazir saab kindly administers them at our house as she is too old to come here,” she says, showering blessings on him. “We don’t find a doctor there [at the NTPHC],” adds Dar, a homemaker and farmer; her husband is a farmer and also rows a shikara on Dal Lake. “They only give polio drops to kids and no one is there after 4 in the afternoon.”
People living on islands on the lake can’t recall seeing a doctor at the primary health centre (NTPHC) for nearly two years – since the consecutive curfews and lockdowns that began in Kashmir in August 2019. “There used to be a doctor there some years ago who did good work, but he was transferred. We haven’t seen one there since 2019,” says Mohammad Rafiq Malla, 40, who lives nearby and works as a tourist photographer. “They [the staff] don’t come regularly and then don’t remain there for enough hours.”
All ‘New Type PHCs’ (‘upgraded’ sub-centres in Kashmir), according to the office of the Assistant Director Planning of the Chief Medical Officer, Srinagar, should have at least one MBBS doctor as medical officer, one pharmacist, one FMPHW (female multi-purpose health worker) and one nursing orderly, all employed by the Directorate of Health Services.


Lake residents can’t recall seeing a doctor at the primary health centre (NTPHC) for two years; an adjacent shed has some medical supplies and discarded furniture
“But the centre only comes alive during [polio] immunisation drives when they make announcements on loudspeakers,” says Wasim Raja, 25, who works on a tourist boat as a photographer, and resides in the same mohalla as the NTPHC (which actually is in Kooli Mohalla, though its board mentions an adjacent locality). “The pharmacist would come home to administer a drip to my father whenever he could,” he adds. “But when we need this dispensary most, it is closed. We then have to go to Nazir or Bilal [another chemist-clinician] or try to reach the road to get to a hospital. It takes time and can be very difficult during an emergency.”
The nearest state-run general hospital, the Jawaharlal Nehru Memorial Hospital in the Rainawari locality of Srinagar, is a 15-minute boat ride from Kooli Mohalla to Boulevard Road, and then two bus rides. Or lake residents have to take a 40-minute boat ride to another point and then walk for around 15 minutes to reach the hospital. In the long biting winters of Kashmir, these journeys can be especially difficult.
Besides the barely-functioning NTPHC, for the roughly 50,000-60,000 people who live on multiple islands in the 18-20 square kilometre Dal Lake, the only other state-run health facility is an ISM (Indian system of medicines) dispensary in Nandpora. It’s at one end of the large water body, and there too the healthcare workers are not always available. And there is a sub-centre on Boulevard Road on the shore (this is also the nearest point for people living on the islands to get Covid-19 vaccines and tests done).
So for the residents of the lake, especially those living on its interior islands, the services offered by Nazir and at least three others who run similar pharmacies – and double up as ‘doctors’ or medical advisers – are often their only accessible healthcare option.
Nazir Ahmad Bhat, who is around 50, and has been working in Dal Lake for about 15-20 years, is available at his shop-clinic in two shifts from 10 a.m. to 10 p.m., with an afternoon break. He says he sees 15-20 patients a day, mainly with ailments like common fevers and coughs, blood pressure issues, persistent pain and minor wounds that require cleaning and bandaging. (He does not tell me about his medical or pharmacist qualifications). Nazir does not take a consultation fee but charges for the medicine at retail price (and derives his income from that), and also stocks medicines for people who need them regularly.

Left: Mohammad Sidiq Chachoo, who sells leather goods to tourists, says, 'We prefer these clinics because they are nearby and have medicines readily available'. Right: The chemist-clinic he is visiting is run by Bilal Ahmad Bhat
At another chemist-clinic nearby, 65-year-old Mohammad Sidiq Chachoo, who sells leather goods to tourists, is getting his blood pressure checked. He has recently been through a gall-bladder removal surgery at a private hospital in Srinagar. "The dispensary [NTPHC] is useless. No one goes there. We prefer these clinics because they are nearby and have medicines readily available," he says.
The clinic Chachoo is visiting is run by Bilal Ahmad Bhat, who lives in Nowgam, on the southern outskirts of Srinagar. He is a licensed chemist and druggist, he tells me, pulling out his certificate given by the Jammu and Kashmir Pharmacy Council.
At his shop – with plywood cupboards containing medicines and a bed for patients to lie down on – from 11 in the morning to 7 in the evening, Bhat says he sees around 10 to 25 patients, most of whom come to him with minor complaints. He too does not charge consultation fees, and only sells the medicines at MRP.
He emphasises that Dal Lake needs a hospital. “There should be at least a gynaecologist here, a maternity mini-hospital where women can get the services required. There are no facilities here for medicals tests. People should at least be able to get their blood sugar checked, their CBC test done. Most of the people here are labourers, they are poor. If they had these facilities at the dispensary [NTPHC] they wouldn't have to come to me for even a Rs. 5 tablet in the cold winters."
Earlier that day, Bilal has had to check on a cancer patient at his home in Kooli Mohalla. “He is undergoing treatment at SKIMS and I had to administer a drip,” he says, referring to the Sher-i-Kashmir institute of Medical Sciences in Srinagar, around 10 kilometres from the Nehru Park
ghat
on the eastern shore of the lake. “I had to close the shop for that duration. He is a poor man who used to row a
shikara
, I couldn't charge him.”


For people living in the Lake's mohallas, the services offered by Nazir and at least three others who run similar pharmacies – and double up as ‘doctors’ or medical advisers – are often their only accessible healthcare option
After dusk, with the NTPHC closing at 4 p.m., people on the lake are even more dependent on the chemists-clinicians. “I get calls in the night when I am at my house,” Bilal says, and recalls an incident when the family of an elderly woman called saying she was breathless. She had been through a surgery at a hospital in Srinagar, and Bilal says, is diabetic and has cardiac problems as well. “When they called me past midnight, I suspected that she might be having a cardiac arrest and advised them [on the phone] to take her to a hospital at the earliest. They did, and it was diagnosed as a stroke. Fortunately, she was saved.”
Deeper into the interiors of the lake, on islands absent from press reports and picturesque photos, the problems can become more acute. During the cold winter months this means breaking six-inch thick sheets of ice to move boats forward a few feet. A ride that will take 30 minutes in summer can stretch to more than three hours when the lake is frozen.
"We need a facility which has doctors during the day and night,” says 24-year-old Hadisa Bhat, who lives in Tind Mohalla in these interiors. “We must also have testing facilities. During the day or even till late in the evening we go to Nazir's clinic. But if someone falls sick during the night, we have to reach for a boat and an oar and take them to Rainawari. An adult might even be able to wait the night out, a child can't,” adds Hadisa, a homemaker, whose four brothers work as farmers or shikarawallas in the lake, depending on the season.
In March 2021, when her mother had a fall and a possible bone injury, she had to be taken to the state-run Bone and Joint hospital in Barzulla in south Srinagar, roughly 8 kilometres from Nehru Park. “Though her injury was not serious, just to get there took us two hours [and autorickshaw and taxi fares],” says Abid Hussain Bhat, Hadisa’s brother. “We made two more trips to the hospital later as there are no facilities nearby which could treat her.”
To try and address at least the problem of ferrying people to hospital from the lake, in December 2020, Tariq Ahmad Patloo, a houseboat-owner, repurposed a shikara into a waterborne ambulance. Media reports at the time spoke of what brought this about – his aunt's fatal heart attack, his own Covid-19 infection. He got financial help from a Trust, and the ambulance now has a stretcher, a wheelchair, an oxygen cylinder, first aid kit, masks, glucometer, and a blood pressure monitor. Patloo, 50, says he is hoping to soon bring on board a paramedic and a doctor. He estimates the ambulance has taken 30 patients so far to hospitals, and has also helped carry dead bodies across the lake.

Tariq Ahmad Patloo, houseboat owner who turned a shikara into a 'lake ambulance'
On their part, the health authorities in Srinagar too are struggling. A senior official, when asked about the paltry facilities in Dal Lake, points to the shortage of staff at his hospital in Khanyar in Srinagar. After the district hospital (the Jawaharlal Nehru Memorial Hospital in Rainawari) was converted into a dedicated Covid-19 facility in March 2020, he says, it brought many non-Covid patients to his hospital, which wasn’t provided additional staff to handle the huge rise in numbers. “If on a typical day we used to get 300 patients, now we have 800-900, even 1,500 some days,” he had told me in January this year.
To prioritise bigger ailments over the seemingly smaller needs of the residents of the lake, the official says staff from NTPHCs and sub-centres has been called to do more night duty than usual, often at continuous stretches, which is why the pharmacist at the NTPHC in Kooli Mohalla has been missing frequently. The FMPHWs, besides their work at health centres, have been crucial in contact tracing during Covid-19, and they too are overworked.
Iftikhar Ahmad Wafai, the 50-year-old pharmacist at the Kooli Mohalla NTPHC for over 10 years, says he is called for night duty at the hospital in Khanyar five times a month, and is unable to report to the NTPHC the next morning. “We aren’t paid extra for this, but we do it,” he says. “We know all facilities are short-staffed and this pandemic has pushed the limits.”
The NTPHC, he adds, has not been allocated a doctor in almost three years. He tried to raise the issue of staff shortage but was told to ‘adjust’. “I even clean the centre myself. I also give injections to patients sometimes, at times I check their blood pressure when they insist,” Wafai says, explaining that this is beyond his job description. “But a patient may not understand that, and you want to help in any way you can.”
And with even Wafai often not available, people living in Dal Lake usually go past the shut NTPHC and onwards to the chemist-clinics where that offer them help when they need it the most.



